Foot Drop
Introduction
Foot drop is a deceptively simple name for a potentially complex problem. Foot drop can be associated with a variety of conditions such as dorsiflexor injuries, peripheral nerve injuries, stroke, neuropathies, drug toxicities, or diabetes.
The causes of foot drop may be divided into 3 general categories: neurologic, muscular, and anatomic. These causes may overlap. Treatment is variable and is directed at the specific cause.
History of the Procedure
Foot drop likely has been a problem for humans throughout our existence. Argument can be made that the biblical story of Jacob limping after wrestling with an angel in the book of Genesis represents the first recorded occurrence of foot drop.1
Problem
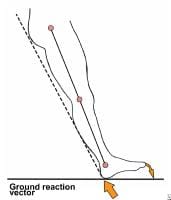
Foot drop can be defined as a significant weakness of ankle and toe dorsiflexion. The foot and ankle dorsiflexors include the tibialis anterior, extensor hallucis longus, and extensor digitorum longus. These muscles help the body clear the foot during swing phase and control plantar flexion of the foot on heel strike. Weakness in this group of muscles results in an equinovarus deformity. This is sometimes referred to as steppage gait, because the patient tends to walk with an exaggerated flexion of the hip and knee to prevent the toes from catching on the ground during swing phase. During gait, the force of heel strike exceeds body weight, and the direction of the ground reaction vector passes behind the ankle and knee center (see image below).
This causes the foot to plantar flex and, if uncontrolled, to slap the ground. Ordinarily, eccentric lengthening of the anterior tibialis, which controls plantar flexion, absorbs the shock of heel strike. Foot drop can result if there is injury to the dorsiflexors or to any point along the neural pathways that supply them.
Frequency
Peroneal neuropathy caused by compression at the fibular head is the most common compressive neuropathy in the lower extremity. Foot drop is its most notable symptom. All age groups are affected equally, but it is more common in males (male-to-female ratio, 2.8:1). Ninety percent of peroneal lesions are unilateral, and they can affect the right or left side with equal frequency.
A foot drop of particular concern to orthopedic surgeons is a peroneal nerve palsy seen after total knee arthroplastyor proximal tibial osteotomy. The estimated rates of this complication are 0.3-4% after total knee arthroplasty and 3-13% after proximal tibial osteotomy. Ischemia, mechanical irritation, traction, crush injury, and laceration can cause intraoperative injury to the peroneal nerve. Correction of a severe valgus or flexion deformity also has been suggested to stretch the peroneal nerve and lead to palsy. Postoperative causes of peroneal nerve palsy include hematoma or constrictive dressings.
In a study by Cohen et al, the relative risk of palsy was 2.8 times greater for patients who had received epidural anesthesia for total knee arthroplasty than for those who received general or spinal anesthesia.2 One postulation is that epidural anesthesia likely decreased proprioception and sensation, continuing to some extent postoperatively, allowing the limb to rest in an unprotected state susceptible to local compression. In addition, intraoperative neurologic damage may not have been readily apparent in the immediate postoperative period because of ongoing effects of epidural anesthesia. In this same study, the relative risk of palsy was 6.5 times greater in patients who had a prior lumbar laminectomy.
A series of patients who developed foot drop following primary hip arthroplasty were carefully examined and found to have spinal stenosis.3 Up to 70% of patients undergoing hip arthroplasty have electromyographic evidence of nerve injury, but they rarely have clinical symptoms.4 Patients with preexisting spinal stenosis are believed to be at increased risk for foot drop following hip arthroplasty because of this proximal compromise. This is the double-crush phenomenon described in more detail in the Pathophysiology section.
Etiology
Foot drop may follow direct injury to the dorsiflexors. A few cases of rupture of the tibialis anterior tendon leading to foot drop and suspicion of peroneal nerve palsy have been reported. This subcutaneous tendon rupture usually occurs after a minor trauma with the foot in plantar flexion.Compartment syndromes also may lead to foot drop. These are surgical emergencies and are not associated only with fracture or acute trauma. March gangrene, a form of anterior compartment syndrome, is thought to be due to edema and small hemorrhages in the muscles of the anterior compartment occurring after strenuous activity in individuals not accustomed to it. Deep posterior compartment syndrome also may result in foot drop as a late sequela due to resultant contracture formation.
Neurologic causes of foot drop include mononeuropathies of the deep peroneal, common peroneal, or sciatic nerves. Lumbosacral plexopathy, lumbar radiculopathy, motor neuron disease, or parasagittal cortical or subcortical cerebral lesions also can manifest as foot drop. These lesions can be differentiated through clinical and electrodiagnostic examinations.
A common behavioral cause of foot drop is habitual crossing of the legs.5 These cases typically resolve with discontinuation of the habit.
Foot drop also may be seen as a combination of neurologic, muscular, and anatomic dysfunction. Charcot foot is one example.
Foot drop also may be seen as a combination of neurologic, muscular, and anatomic dysfunction. Charcot foot is one example.
Pathophysiology
The pathophysiology of nerve damage commonly causing foot drop is as follows:- The functional integrity of an axon and its target depend on the continued supply of trophic substances synthesized in the neuronal perikaryon and transported down the axon, known as axoplasmic flow.
- A laceration interrupts this flow. A crush injury may compromise it as well.
- A double-crush phenomenon occurs when a proximal insult in a nerve root diminishes axoplasmic flow, making it more susceptible to injury.
- A distal lesion further compromises the flow, and clinical palsy results. This is the phenomenon thought to be responsible for the increased risk of foot drop after hip replacement in a patient with preexisting spinal stenosis. The spinal stenosis causes the proximal compromise, and intraoperative stretch of the sciatic nerve provides the distal insult.
Presentation
Direct injury to the dorsiflexors
With dorsiflexor injury due to laceration or contusion, both cause and effect are readily apparent on clinical examination. A young healthy or active healthy elderly patient usually benefits from surgical repair of the injury.
If the patient develops a degenerative rupture of the tibialis anterior muscle, foot drop may be observed, but the cause may not be immediately apparent. Such a patient is often an elderly man who suffers a minor trauma with the foot in plantar flexion. The patient stands with the foot everted and has some loss of dorsiflexion when attempting to heel-walk. The degree of foot drop varies depending on time elapsed since the rupture. Active function in the other muscles innervated by the deep and superficial branches of the peroneal nerve essentially rule out the possibility of a peripheral neuropathy. Functional recovery is achieved over time and is aided by bracing of the affected ankle. Surgery may not be required in this situation.
Compartment syndromes
Increased pain with passive stretch of the involved muscles is a consistent diagnostic indicator of a compartment syndrome. Pain out of proportion to the injury usually is the initial presenting symptom. Paresthesias follow, but at this point, irreversible myoneural injury has likely occurred. Foot drop also may be noted; the time of presentation varies with the compartment involved.
- Anterior compartment syndrome
- Clinical presentation of an acute anterior compartment syndrome includes pain with passive toe flexion, some weakness of toe extension, and diminished sensation in the first web space because of deep peroneal nerve compression.
- The extensor hallucis longus usually is the first muscle to show weakness.
- Anterior compartment syndrome may follow trauma to the extremity but also can be observed in march gangrene. Local erythema, heat, and brawny edema over the anterior compartment are present.
- Regardless of the cause, wide fasciotomy of the anterior compartment must be performed to salvage the ischemic muscles.
- Deep posterior compartment syndrome
- An acute deep posterior compartment syndrome presents as pain and some weakness of toe flexion and ankle inversion. Pain on passive toe extension is referred to the calf.
- Diminished sensation over the sole of the foot especially on the medial side is noted, resulting from posterior tibial nerve compression.
- Foot drop develops because of ischemic contracture of the posterior compartment and is seen if the acute syndrome is not treated.
- Once again, wide fasciotomy of the involved compartment is mandatory at the time of acute presentation.
- Chronic compartment syndrome
- This occurs in athletes in their third or fourth decade who have exercise-induced pain in the lower leg or foot within 20-30 minutes of beginning to exercise. Often, this occurs after a recent increase in intensity or duration of training or after a change in the training routine.
- The symptoms resolve after 15-30 minutes of rest; however, as the syndrome progresses, pain occurs earlier and takes longer to resolve.
- The anterior compartment is the most commonly involved.
- Unless the patient has been exercising just before being examined, the physical examination may be nonspecific or normal.
- Patients with a chronic anterior compartment syndrome may have diminished sensation in the first dorsal web space.
- Recording of intracompartmental pressures before, during, and after exercise can provide useful diagnostic information as to which compartments may be involved. The following are believed to be indicative of the syndrome: a resting pressure of 15 mm Hg or more and/or a pressure of 30 mm Hg or more 1 minute post exercise and/or a pressure of 20 mm Hg or more 5 minutes post exercise. A slit catheter may be used to measure these pressures with the understanding that accuracy of the readings is influenced by depth of needle insertion; position of the leg, ankle, and foot; and force of muscle contraction.
- Some preliminary investigation has been completed of MRI as a potential test for chronic compartment syndrome.
- Nonsurgical treatment of a chronic compartment syndrome is only successful if the patient is willing to discontinue the inciting activity. The surgical treatment of choice is fasciotomy of the involved compartment.
Neurologic defects
Several neurologic defects can cause foot drop (see Introduction, Etiology). Equinovarus deformity associated with toe contracture is the most common lower extremity manifestation of stroke. This can be differentiated from a peripheral neuropathy on examination by eliciting hyperactive deep tendon reflexes and a positive Babinski sign. The patient's gait pattern can also suggest etiology. For example, patients with a paretic foot drop bear weight on the heel during initial foot strike, whereas those with a spastic deformity strike with the forefoot.
Another central nerve insult that can be associated with foot drop is L5 compression. In addition to weakness in the peroneal nerve distribution, the tibialis posterior is weak. Back pain, sciatica, and limitation of straight leg raising also are seen. Motor conduction velocity may remain normal.
Peroneal neuropathy also may be spontaneous, traumatic, or, less frequently, progressive. Peroneal neuropathy is characterized by weakness in dorsiflexion without back pain, sciatica, or other symptoms. Leprosy neuritis, for example, affects nerves where they are close to the skin and pass through a narrow fibrous or osseous canal. In addition to peroneal nerve palsy, patients with leprosy may have involvement of the posterior tibial nerve at the tarsal tunnel leading to anesthesia of the sole of the foot.
Foot drop from neuropathy may develop in patients who have undergone bariatric surgery, especially those who experience rapid postoperative weight loss.6 Micronutrient deficiencies (eg, vitamin B-12) may be a factor in these cases.7
Foot drop from neuropathy may develop in patients who have undergone bariatric surgery, especially those who experience rapid postoperative weight loss.6 Micronutrient deficiencies (eg, vitamin B-12) may be a factor in these cases.7
Combination of neurologic, muscular, and anatomic dysfunction
These patients typically are diabetic and develop loss of protective sensation and proprioception, leading to unperceived trauma. This is coupled with an autonomic neuropathy that results in loss of sympathetic vasoconstriction and enhanced pedal blood flow, causing demineralization and subsequent bone weakness. Unperceived trauma, demineralization, and bone weakness culminate in destruction of the tarsal bones. This, in turn, forms a bony block at the ankle joint and foot drop. Progressive motor neuropathy is also present, in which the muscles weaken distally to proximally, resulting in loss of strength in the anterior compartment. The anterior muscles are overpowered by the Achilles tendon, leading to abnormal pronator stress at the midtarsal joint, further encouraging osseous breakdown and foot drop.
Relevant Anatomy
Fibers from the dorsal branches of the ventral rami of L4-S1 are found in the peroneal nerve, which is paired with the tibial nerve to constitute the sciatic nerve. The sciatic nerve leaves the pelvic cavity at the greater sciatic foramen, just inferior to the piriformis muscle.
The sciatic nerve bifurcates to form the peroneal and tibial nerves either at the distal third or mid-thigh level. The peroneal nerve crosses laterally to curve over the posterior rim of the fibular neck to the anterior compartment of the lower leg, dividing into superficial and deep branches. The superficial branch travels between the 2 heads of the peronei and continues down the lower leg to lie between the peroneal tendon and the lateral edge of the gastrocnemius. It then branches to the ankle anterolaterally to supply sensation to the dorsum of the foot (see image below).
The deep branch divides just after rounding the fibular neck. The initial branch supplies the anterior tibial muscle. Remaining branches supply the extensor digitorum longus and extensor hallucis longus and a small sensory patch at the first dorsal web space (see image below).
The peroneal nerve is susceptible to injury all along its course. As part of the sciatic nerve, its funiculi are relatively isolated from those of the tibial nerve. Therefore, trauma to the sciatic nerve may only affect one of its divisions. Also, the funiculi of the peroneal nerve are larger and have less protective connective tissue, making the peroneal nerve more susceptible to trauma. In addition, the peroneal nerve has fewer autonomic fibers, so in any injury, motor and sensory fibers bear the brunt of the trauma. The peroneal nerve runs a more superficial course, especially at the fibular neck, also making it vulnerable to direct insult. It adheres closely to the periosteum of the proximal fibula, making it susceptible to injury during surgical procedures in this area
.
.


Best Dual Channel Pain relief Device tens unit electronic pulse massager for Chronic pain like back pain, Neck pain, Lower pain, Solder pain, period cramp pain and so on..
ReplyDeleteيمكن اعتبار تركيب طارد الحمام وسيلة فعّالة لمنع الحمام من التراص على المباني أو الشرفات، وذلك لتجنب الأضرار الناتجة عن مخلفاتها. فيما يلي بعض
ReplyDeleteالخطوات الأساسية لتركيب طارد الحمام:
تركيب طارد الحمام بالرياض
بيع طارد حمام بالرياض