LOW BACK PAIN
DEFINITION
Pain on the lumbar area caused by an underlying disease. It is not a disease but a symptom. Pain between the costal margins and gluteal folds.
Anatomy
· The kidney shaped lumbar vertebral body is wider laterally than it is deep anteroposteriorly, and broader than it is high. Its periphery is deeply hollowed out in a shape of a diabolo, except posteriorly where it is nearly flat.
· The two (2) laminae are highly set and run posteriorly and medially but they lie in a plane which is oblique inferiorly and laterally.
· The transverse processes, better called ostiod process since they are in fact rib vestiges.
· They are attached at the level of the articular processes and run an oblique course posteriorly and laterally.
· The pedicle, a short and bony segment joining the vertebral body to the vertebral arch and attached to the former at its superolateral angle.
· The superior articular process lies on the superior border of the vertebral arch near the junction of the lamina with the spinous process.
· The vertebral body of L5 is higher anteriorly than posteriorly so that its profile is wedge-shaped or even trapezoidal with its longer side lying anteriorly.
Spine
· An aggregate of superimposed segments that can be termed functional units.
Functional Unit:
· Composed of two vertebral bodies, one superincumbent on the other, separated by the IV disk.
Anterior weight bearing portion of the functional unit:
· Comprised of two adjacent rounded vertebral flattened at their cephalad and caudal ends.
· At birth and throughout maturation, caudal and cephalic ends of the vertebra are slightly convex and coated with cartilage, undergoes ossification from age 15-20 and fuse with the vertebral bodies.
· Ossification layer at each endplate called epiphysis, remains active throughout growth; influence by Wolff’s law
Intervertebral disk
· 80% of load
· Hydrodynamic elastic structure that is imposed between two adjacent vertebrae; shock absorbing mechanism
· 25% height of the spine
· 90% composed of water- decrease with age
· 65% water in old age
· Central (nucleus) pulposus:
o Ovoid, yellowish and gelatinous in appearance
o Middle part of the IV disk
o Made of mucoprotein
o Proteoglygcans- responsible for water retention
§ Greater than collagen
· Annulus fibrosus
o 20 firm, concentric rings of collagen surrounding the nucleus pulposus
o 3 layers of fibrocartilage:
§ Sharpey’s fiber- outermost layer
o Collagen > proteoglycans
· Nucleus- homogenous, elastic globoid centrally located within a fibrocartilagenous envelope most disk hydration occurs via imbibition.
· The disk in early human development is nourished by direct blood supply; upon maturation, nutrition is by primarily imbibitions, and to a lesser extent, osmosis.
· Annular fibers fail after exceeding 5 degrees of rotation, site of failure varies because of the differences in angulation where the inner fibers have more vertical orientation.
Posterior portion of the functional unit:
· 20% of load
· Forms the outer wall of the spinal canal
· Neural arch extends posteriorly as pedicles to form as lateral transverse process
· Widens to form the zygaphophyseal(facet) joint (note that the lumbar zygapophysis lie I the sagittal plane, which allows flexion and extension, markedly restricts rotation and lateral flexion)
· Laminae continues postermedially to rejoin centrally and form the posterior superior spine
40-50% of the torque strength of the whole joint is providedby the disk annulus, the rest is provided by the posterior articulations: (the facets, their capsules and interspinous ligament)
*as the lumbar spine laterally flexes, there is mandatory, simultaneous rotation toward the side that the spine bends:
1. facets of the concave side approximate
2. facets on the side from which the spine is bending separate
3. IV disk is sheared laterally with a degree of rotation
4. normal movement does not change the width or the content of the foraminal to an abnormal unphysiologic degree
Ligaments of the Lumbar Spine
In the sagittal section there are two (2) sets of ligaments:
· The anterior longitudinal ligament- stretches as a long dense band from the base of the occiput to the sacrum on the anterior aspect of the vertebrae.
· The posterior longitudinal ligament- stretches from the base of the occiput to the sacral canal. It tapers at the level of L2 ( reason why posterolateral herniation is more common)
Segmental ligaments that joins the vertebral arches:
· Ligament Flavum- inserted inferiorly into the superior border of the underlying lamina and superiorly into the medial aspect of the overlying lamina.
· Interspinous ligament
· Supraspinous ligament
· Intertransverse ligament
Muscles
Erector Spinae (sacrospinalis)
Origin: last 2 thoracic vertebrae, lumbar vertebrae, sacral spine, sacrum, SI ligament, medial aspect of the iliac crest.
Spilts into three(3) columns:
· Iliocostalis (lateral)- inserts into the angle of the rib cage (C4-T6)
· Longissimus- inserts in the transverse processes cephalad to T1 (only one to reach the skull)
· Spinalis(medial)- flat, aponeurosis muscle. Insertion at the posterior spine of the thoracic vertebrae
Transverse Spinae (underneath the erector spinae)
1. Semispinalis ( superficial)- origin: tips of the transverse processes
Insertion: tips of the posterior spinous process; Spans 3-5 segments
2. Multifundus- between the spinous and transverses crest, from overlying erector spinae aponeurosis and from all the transverse processes up to C4 vertebra
-spans 3 vertebral segment- attach to the superior border of the next transverse process above it.
3. Rotatores- spans only one segment; origin: transverse process of one vertebrae to the spinous process of the adjacent vertebrae.
Other muscles:
1. interspinalis- between two adjacent spinous process
2. intertransversii- between adjacent transverse process
Thoracolumbar fascia
· deep investing membrane which covers the deep muscles of the back of the trunk. It is made up of three layers, anterior, middle, and posterior. The anterior layer is the thinnest and the posterior layer is the thickest. Two spaces are formed between these three layers of the fascia. Between the anterior and middle layer lies the quadratus lumborum muscle. The erector spinae muscle is enclosed between the middle and posterior layers.
Angles of the Lumbar Vertebrae:
1. Angle of the sacrum- approximately 30 degrees
- measured from the horizontal line toward the superior surface of S1.
2. Angle of Pelvic Tilt- approximately 60 degrees
- from the horizontal line across the line within the promontory of sacrum and symphisis.
3. Lumosacral angle- approximately 30 degrees
- angle from the axis of L5 to S1
Lumbar pelvic Rhythm
· It is the coordinated movement of the lumbar spine and pelvis
· The lumbar spine has 5 functional units, each unit flexes approximately 9 degrees (5 units= 45degrees), allowing the person to bend over forward only a portion of the amount of flexion required for toe touching.
· For additional forward flexion, a simultaneous rotation of the pelvis must occur.
· Sequence of activities occurring within the functional units:
a. during flexion:
1. extensor muscle relaxed and 3 physiologic curves becomes straight
2. upon flexion head moves ahead of the COG, there is contraction of the erector spinae muscles
3. further forward flexion, lumbosacral spine goes to kyphosis.
4. extensor muscles elongates smoothly and gradually.
5. erector spinae muscles goes eccentric contraction, each functional unit flexes about 9 degrees
6. hip extensors maintain isometric contraction
7. when back muscles and ligament become taut, full lumbar khyphosis has been reached.
8. pelvis begin forward rotation by elongation and deceleration of gluteus maximus and hamstrings to give further way to flexion
9. full flexion has been achieved, the pelvis is stricted by its ligaments and facial tissue.
10. no muscular activity, only fascia and ligaments are operative.
b. during re-extension:
1. pelvis should rotate first before the lumbar spine resumes its lordosis.
2. the hips and the knees should be slightly flexed.
3. resumption of the erect posture without excessive rotation and de-rotation.
Pain Free structures:
1. IV disk (nucleus pulposus, inner and middle layer of annulus fibrosus)
2. Vertebral body
3. nerve root (per se)- irritation will only cause paresthesia, dysthesia, paresis but rarely pain
4. Ligamentum Flavum
Pain sensitive structures:
1. outer layers of annulus fibrosus
2. Anterior Longitudinal Ligament
3. Posterior Longitudinal Ligament
4. Recurrent nerve from nerve root
5. Erector Spinae
6. Other posterior supporting ligaments
7. Zygapophyseal joints
Disc Pressure in various postures:
Supine 25%
Side lying 75%
Standing Upright 100%
Sitting upright 140%
Standing while bending forward 160%
Sitting while bending forward 185%
Standing while bending forward
and holding weights 220%
Sitting while bending forward
and holding weights 275%
Types of Low Back Pain:
1. Static LBP
· Excessive lordosis or “sway back” posture has been considered and is responsible for 75% of all static or postural LBP
· Pain is produced by:
o Approximation of the facets with compression
o Intervertebral foramen closes and encroaches the nerve root dura
o Disk can bulge posterolaterally, putting the strain on the posterior longitudinal ligament
· When approximation of the post articulation causes sliding of the facets (kissing of the spine) into each other, they become weight bearing which is not its physiologic function, resulting in synovial inflammation leading to pain.
· Excessive lordosis is usually seen in:
o Pregnant women who stand with arched back
o Improper sitting position
o Persons wearing high heeled shoes
o People with poor sleeping habits (prone positioning)
o Occupation requiring hours of sitting and standing (i.e delivery truck drivers, people who do ironing)
2. Kinetic Low Back Pain
· Implies irritation of pain- sensitive tissues activated by movement of the spine
· Caused by improper functional use of lumbosacral spine
· Impaired lumbar pelvic rhythm
· Pain can originate in these manners:
o Normal stress on an unprepared back
§ Lack of anticipation and preparation causing contradiction to “overshoot the mark”
§ Excessive movement exceeds the physiologic limitation imposed by the ligaments
§ Micro or macocapsular and articular tissue damage occurs resulting in pain and disability
o Abnormal stress on a normal low back
§ By extraordinary weight imposed on the supporting structure
§ By average weight held in a markedly eccentric manner
§ By light object held for unduly lone period of time
ü Forward flexed standing or sitting posture of 10 -15 degrees
§ Cause of industrial cases of LBP
o Normal stress on an abnormal low back
§ Conditions such as structural scoliosis, tight hamstrings, and osteoarthritis
EPIDEMIOLOGY
ü Second to headache as leading cause of pain
ü Leading cause of expense in workers compensation
ü 60-90% lifetime rate
ü >5 % annual rate
ü Men=women
ü >1% with lumbar radiculopathy
ü Age of lumbar surgery=45
ü 5th highest reason of hospitalization
ü Most episodes resolve with or without treatment
ETIOLOGY
A. Congenital disorders
o Sacralization of lumbar vertebrae
o Lumbarization of sacral vertebrae
o Tropism
§ Assymetrical segmental scoliosis usually in the lower lumbar segments
§ Nerve root on the side of concavity prone to entrapment
§ L4-L5, L5-S1
§ Back area may present with tenderness upon palpation
§ Radicular pain
§ Paresthesia if with nerve root entrapment
§ Agrrevated by extension with lateral flexion to the concave side
§ Relieve with flexion and lateral flexion towards convexity
B. Tumors
o Benign
§ Involving nerve roots of meninges
§ Involving the vertebrae
o Malignant
§ Primary malignant tumors (multiple myeloma-most common)
§ Secondary malignant tumor (metastatic- most common tumor)
- Metastatic cancer from the lungs, prostate, breast, kidneys, and colon.
- Symptoms: pain especially at night
Treatment:
· Radiation therapy
· Decompression bracing
· Ambulatory assistive device
C. Trauma
o Lumbar strain
o Fractures
o Spondylolysis- fracture of the pars interarticularis
- Unilateral
- Commonly involving L5 and L4
- Male> female
Etiology:
§ Stress Fracture
§ Congenital failure of fusion during maturation of the bones
§ Birth fractures
§ Increase lumbar lordosis
§ Impingement of the articular process on the pars interarticularis
§ Weakness of the supporting muscles
§ Pathologic changes in the pars interarticularis
§ Axial loading of only about 600 lbs is sufficient to produce fracture in the isthmus of the neural arch if the spine is maintained in hyper lordosis
Pathophysiology:
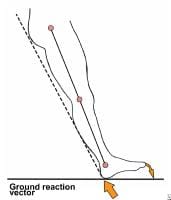
§ The gravitational and muscular loads acting across the step in inclined of the upper surface of the sacrum can be resolved into:
· Shearing components( L5 displaced forward on S1.
· Compressive component
ü at right angles
ü in accordance with Newtons 3rd law
- The mutual forces of action and reaction between two bodies are equal, opposite and collinear. This means that whenever a first body exerts a force F on a second body, the second body exerts a force −F on the first body. F and −F are equal in magnitude and opposite in direction. This law is sometimes referred to as the action-reaction law, with F called the "action" and −F the "reaction".
Signs and symptoms:
§ localized lumbosacral pain that is usually worst with extension and partially relieved with flexion
§ local tenderness
§ spasm
Diagnosis
§ Xray- degenerative and hypertrophic changes can be found
§ CT scan
§ MRI
Treatment
§ Rest
§ Rigid mobilization(e.g. Modified Boston overlap brace)- worn 23 hrs per day for 6 mos in cases of symptomatic spondylolysis
o Spondylolisthesis- forward or backward shearing subluxation of the body of a superior vertebrae on its caudal counterpart
- Most common L5 on S1, and L4 over L5
- Grade according to displacement:
I forward displacement of </= to 25%
II forward displacement of 26-50%
III forward displacement of 51-75%
IV forward displacement of >75%
Etiology:
§ 5th lumbar vertebrae tends to glide forward due to shear force and gravity
§ Forward sliding is normally prevented by mechanical alignment and relationship of posterior facet joints, their ligaments, capsule, integrity of IV disk and of the longitudinal ligaments.
· Intact nucleus pulposus expand the disk and places the annulus fibers and longitudinal ligament under tension that resist vertebral sliding
· The contact of the facets and their planes also resist anterior subluxation of the vertebrae
§ Defect in any of the supporting structures may permit listhesis of the superior vertebrae over the inferior vertebrae of the involved functional unit.
ü 5 categories according to causative factors:
1. Isthmic- most common; occurs due to spondylolysis of the pars interarticularis
2. Dysplastic or congenital- caused by dysplasia of the facet joint of the upper sacrum, leading to inability to resist shear stresses, then forward slippage occurs
3. Degenerative- seen in older spine, related to long standing intersegmental instability from degenerative facet or disk disease; most common in L4 and L5 level.
4. Traumatic- rare; cause by acute fracture secondary to trauma
5. Pathologic- secondary to metabolic and malignant or infectious disease.
§ Other causes:
· Backward bending(e.g. Gymnastics)
· Obesity and disk degeneration
· Congenital asymmetrical facets
Clinical Manifestations:
§ LBP with referred pain laterally to the region of the SI joints
§ Pain radiate to hips, thighs, and even to the feet, not precisely in dermatomal pattern
§ Stiffness with limited flexibility
§ Presence of palpable “ledge” on LS spine
§ Segmental Lordosis
Diagnosis
§ Xray and CT scan may reveal:
· Defect in pars interarticularis
· Elongated arch
· Fracture
· Severe LS angulation
· Severe IV disk degeneration
§ Lateral view of LS spine reveals degree of subluxation
· Foraminae are deformed and sciatic radiculopathy may result
· Normal foraminae narrows during the process of extending the lumbar spine
· Narrowing is enhanced and nerve entrapment is more probable
Treatment
§ Surgery- when there is neurologic deficit
· Anterior interbody fusion between L4-L5 or L5-S1
· Laminectomy- if neural arch is involved
§ PT management
· Pelvic tilting
- Exercise in which ant. aspect of the pelvis is elevated and the posterior lowered
- Strong abdominals, especially the obliques must be gained and maintained
- Avoid excessive lordosis
- Extensor muscle must be strengthened
· Corset or braces
- Decreases lordosis
- Reinforces the abdominal component
- Minimizes excessive motion during lifting and bending
- Must be used as an adjunct to exercise not to replace it.
D. Metabolic Disorder
o Osteoporosis- decrease bone mass per unit volume of bone
o Osteomalacia- disturbance in calcium metabolism
E. Inflammatory Diseases
o Rheumatoid arthritis
o Ankylosing spondylitis (bamboo spine)
Ø Marie strumpell- ascending
Ø Bechterew- descending
F. Degenerative Disorder
o Spondylosis- kissing of spine
§ Degenerative or osteoarthritic changes in the spine
§ Stiffness is the main feature
§ Dull and nagging pain and stiffness in the morning
§ Treated by resting
§ Induced by lumbar extension
Treatment:
§ avoid hyperextension
§ weight control
§ isometric exercise of the quadratus lumborum and abdominals
§ avoid sleeping prone
§ LS support for severe pain( avoid use >3 weeks)
§ NSAIDS
§ Facet joints injection
o Osteoarthritis- wear and tear
o Herniated disk- disk protrudes backward and compresses the nerves that are distributed to the LE.
- 90% occurs in the region of L4-L5, L5-S1 disk spaces
- Found I patients between 30-50 y.o
Types:
a. Protrusion
- Most common
- Involves no tearing of the annulus fibrosus with some bulging of the nucleus pulposus
b. Prolapse
- Complete tear through the annulus fibrosus but with an intact anterior &/or posterior longitudinal ligament
- Only the outermost fibers of the annulus contains nucleus
c. Extrusion
- Complete tear through the annulus fibrosus with involvement of the longitudinal ligaments
- Annulus fibrosus is perforated and discal materials moves into the epidural space
d. Sequestration
- Formation of discal fragment from the annulus fibrosus and nucleus pulposus outside the disk proper.
Etiology:
§ Herniation of the nuclear materials usually occurs after the onset of degenerative changes
§ Most rupture occur in the 3rd of 4th decade
§ Rupture result of combination of acute trauma and pre-existing degenerative changes
§ Poor conditioning and faulty biomechanics
Clinical Manifestations:
§ Recurrent episodes of back pain and pain in the lower leg
§ Prolonged sitting or standing can aggrevate the pain
§ (+) sciatic pain/ radicular pain
§ Increase in intra spinal pressure caused by coughing, sneezing, or bending down and during bowel movements
§ Spinal movement also aggrevate the pain
Treatment
§ Surgical
· Laminectomy
· Laminotomy- division of a lamina of a vertebrae
· Nucleotomy
§ Pt management
· Icing for 15 mins (acute onset)
· Heating modalities after 24-48 hrs.
· Intermittent lumbar traction of nerve root pain( pain radiating down the legs)
· PRES on abdominals
· Postural control
· Use of proper body mechanics
· Use of a plaster jacket to provide rest and security to the spine for 3-4 weeks
o Spinal Stenosis- localized narrowing of the spinal canal from the structural abnormality of each bony components
- Canal may be narrowed by reduction of its transverse diameter, AP diameter, or both.
- Narrowing of the central portion of the spinal canal gives rise to central stenosis and the narrowing of the lateral part of the nerve canal.
- Give rise to lateral stenosis with lateral body entrapment
- Greatest central canal narrowing occurs at L3-L4 and L4-L5 regions.
Etiology:
§ Congenital- primary
Ø Idiopathic
Ø Achondroplastic- pedicles are short and the interpediculate space is decreased.
§ Acquired- secondary
Ø Spondylolisthetic- pars interarticularis defect secondary to DJD
Ø Iatrogenic- post diskectomy, post fusion
- Metabolic disease like Paget’s Disease(chronic skeletal disease characterized by progressive structural changes and typical deformities occurring in long bones, spine, pelvis, and cranium.
Pathomechanics
§ Narrowing of the lumbar spinal canal
§ Degenerative changes can lead to further narrowing
§ Lumbar spine becomes stenotic
§ (+) leg pain when walking
Clinical Manifestations:
§ Pseudoclaudication( neurologic claudication)
- Paresthesias of one or both legs occurring after a period of distance walking or after a period of standing.
- Symptoms subsides then disappear after sitting
- As the symptoms gradually progress, weakness of the legs may interfere with normal gait
Factors that lead to pseudoclaudication:
a. Exercise of the legs normally causes an increase venous capacity, dilatation of veins that accompany the nerve roots as they emerge to the foraminal gutters
b. If there is compression of nerves within the foramina, there is arterial supply limitation compromised of the venous return.
§ Sitting flexed forward causes a lumbar kyphosis and the following results:
- canal lengthens
- cauda equina fibers elongates
- facets separate and the foraminae opens
- Venous capacity and blood flow to the nerve returns
Diagnostic procedures:
§ CT scan
-Most effective in identifying spinal stenosis
§ EMG
-Provide additional evidence of nerve root involvement
§ Xray findings:
· Lateral view: shortening of the lower lumbar pedicles
· AP view: reduce distance between pedicles
Differential Diagnosis
| INTERMITTENT CLAUDICATION | PSEUDOCLAUDICATION |
| Pain on calves (distal to proximal) | Pain on lumbar spine – calf |
| Elicited by walking lone distance & exercise | Elicited after prolonged standing |
| Pain is usually felt as squeezing and cramping | Felt as numbness or burning; rarely cramping |
| Relieved by cessation of activities | Relieved by sitting and stooping forward |
Treatment
§ Medical management
Ø Oral steroids and epidural steroids
§ Surgical management
Ø Laminectomy- surgical removal of the lamina
Ø Foraminectomy- surgical removal of the foramen
§ PT Management
§ Williams Exercise- abdominal strengthening
§ Lumbosacral support- ex. Corset
§ Pelvic and Gravity Traction
§ Rest
G. Mechanical Causes
o Intrinsic factors
§ Poor muscle tone
§ Myofascial pain
§ Instable vertebrae
§ Hyperlordosis
o Extrinsic factors
§ Renal problem
§ Hip problem
§ Scoliosis
DIAGNOSIS
A. Clinical
1. History
a. mode of onset
b. aggrevating and relieving factors
c. effect of posture, exertion, rest
d. effect of cough, sneeze, strain
e. presence or absence of pain at night
f. course of pain
g. history of back or lower limb pains
h. associated lower limb symptoms
i. urinary frequency, urgency, retention, bowel/bladder incontinence
j. history of lumbar surgery
k. treatment implemented, medications used, and effects of these medications
l. presence or absence of litigation or compensation issues
2. Examination
· Inspection
a. Deformities
b. Paraspinal spasms
c. Birthmarks
d. Unusual hair growth
e. Listing to one side
f. Decrease or increase lordosis
g. Scoliosis
h. Atrophy
i. Asymmetries
· Palpation and percussion
a. Trigger points
b. Local tenderness
c. Spasm
d. Tightness
e. Withdrawal to touch
· ROM of lumbar spine
a. Flexion- 40 degrees
b. Extension-15degrees
c. Lateral bending- 30 degrees
d. Rotation-40 degrees
· Neurologic Exam
a. Gait and coordination
b. Muscle stretch reflex
c. Muscle bulk
d. Muscle strength
e. Sensory examination
3. Special tests
1. Neurologic Dysfunction
a. SLR/Lasegue test
- Passive flexion of the hip until pain is elicited
- 0-30 degrees- muscular
- 30-70- neuropathic
- >70 degrees- skeletal
b. Brunzinki’s Sign/ Hyndman’s/ Lindner’s/Soto-hall sign
- Flex neck until the chin is on the chest
c. Braggard’s test
- Foot DF
- Pain with neck flexion and foot DF- stretching the dura mater
- Foot DF alone- hamstring tightness
d. Sicard’s test
- SLR and extension of the big toe
e. Turyn’s test
- Extension of the big toe
f. Bilateral SLR
- Pain <70degrees- SI joint lesion
- Pain >70 degrees- Lumbar spine lesion
g. Well leg raising/ Lhermitte’s / Cross over sign
- Space occupying lesion- herniated disk
h. Prone knee bending/ Nachlas test
- Passively flex knee while in prone
- Unilateral lumbar pain- L2-L3 nerve lesion
- Anterior thigh pain- quadriceps tightness
- SI/ lumbar pain- tight rectus femoris
i. Kernig- Brudzinski’s Test
- Flex head unto chest while supine
- Flex hip with legs extended until pain is felt
- Flex knee until pain disappear
- Significance- meningeal, nerve root or dural irritation
2. Test for Spinal Theca Compression
a. Naffzigger’s Test
b. Valsalva’s maneuver
c. Milgram’s test
3. Test for SI pathology
a. Patrick/FABER Test
b. Gaelen’s Test
c. Pelvic Rock Test
4. Test for muscle tightness
a. Thomas Test
b. Ober’s Test
B. Diagnostic Testing
Ø Plain Radiography
· Fracture
· Dislocation
· Spondylolisthesis
· Degenerative disease
· Narrowing of IV disk spaces
· Tumors of he spine
Ø Radiostope Bone Scaning
· Tumors( bone metastasis)
Ø CT scan and MRI
· Disk disease
· Herniated or extruded disk
· Tumors
· CT scan for bony lesion
· MRI for epidural, intradural, intraaxial spinal cord lesion
Ø MRI Electromyography
· Neurogenic changes and denervation
· Provides physiologic exam
DIFFERENTIAL DIAGNOSIS
Rickets
In the presence of a spinal curve that was distinguished by the alteration of the shape in the other bones with which it is accompanied, especially in those in the lower limbs and the chest one could make the diagnosed rickets of rachi is, rickets a wide spread disorder, was sometime referred to as the “depressed of the spine.
Stooped Posture
A” hooped like curvature” could occur in rheumatism, however, a smoothly rounded anterior curvature could also be congenital or developmental. Some people, either from their original conformation or from early habit of stooping, present the appearance of a very considerable gradual or hoop-like curvature.
Tuberculosis
It was especially important to differentiate rheumatism, rickets, and more postural deformities form bony tuberculosis, an infection frequently encountered in those days. Tuberculosis, referred to as scrofula or white swelling, was identified in the spine on the basis of a kyphosis that instead of being smoothly rounded, was interrupted by, an angle projecting posteriorly. Such an angular curvature can be produced into other way, and can never be mistaken.
Syphilis
The other infection disease one had to keep in mind was syphilis, although not as common cause of back pain. It was usually encountered in the skull, tibia or ulna. Pain cases showing skeletal deformities, especially those presenting with a deformed and painful shin bone, were diagnosed as vascular musculo rheumatism resulting in either from a syphilic cause or from the aggressive treatment of syphilis with mercurial drugs, in which case it was known as mercurial rheumatism.
Scoliosis
Known as lateral curvature of the spine, scoliosis was often encountered especially in girls. The direction of the curve made the diagnosis easy.
MEDICAL MANAGEMENT
Medications should be taken 4-6 hours. Taking the medication whenever necessary can cause drug dependency.
· anti-inflammatory drug blocks the transmission of substances that could imitate soft of the low back.
· NSAIDS provide anti-prostaglandin B formation
· steroids for severe pain
· muscle relaxant muscular tension compresses all the inflammed tissues and restricts movements which cause pain but is questionable since muscle spasm is protective in nature
· sedative tranquilizer
· anti-depressant endorphin formation
· intramuscular injections and injection of an anesthetic agent with soluble steroid injected into the multifidus triangle which frequently interrupts the painful low back pain
SURGICAL MANAGEMENT
Surgical approach and techniques are indicated assuming that:
· patient has been correctly selected as suitable operation
· proper conservative treatments has failed
Approaches can be subdivided into:
Anterior Trans operational app.
· used for 1.5 SI fusion
· also used osteomyelitis and tumors involving L5-S1
· can't be used in decompressing the neural elements
Anterior Intra operational app.
· provides a wide exposure
· all operation involving the vertebral body and disc from L2-S1
· better for L4-5 and L5-S1 fusion
· advantage iliac grafts can be taken through the same skin incision
· posterior midline app.
· all posterior elements, transverse processes, spinal canal, disc spaces and vertebral bodies and be exposed for surgical techniques enumerated below.
To operate merely to relieve pain is not and should not be an indication for surgery. Fear in the mind that pain is very subjective
1) Laminectomy and/or Laminetomy
- is the surgical approach to seeing and ultimtely removing the osteophytes
- laminetomy implies removing asufficient portion of the lamina to view the nerve within the neural canal or within the foramen
- laminectomy implies removing all the half of the lamina thus giving the target view of the nerves of wider in the neural canal to free the nerve roots
2) Foraminectomy
- is a technique of widening of foramena that has been confirm to be narrow or deform bone thus being too narrow for the emerging nerve root
PHYSICAL THERAPY MANAGEMENT
Goals of final rehabilitation
· Full, pain free ROM of the injured and adjacent ligaments as well as hip, girdle, spinal and lower extremity structures that influence the lumbar spine.
· Optimal strength, endurance and coordination of the neuromuscular system affecting the lumbar spine.
· Prevention of further injury and recurrence
· Return to normal functional activities
Acute phase goal
§ decrease pain and inflammation
§ protect injured area from further injury
Subacute phase goals
§ regain soft tissue flexibility and segment motion
§ restore full function to injured and supporting structures
§ maximize lower extremity muscular flexibility for normal lumbar motion
§ optimal joint mobility
Chronic phase goals
§ multidisciplinary pain management
§ improve functional ADL's
§ discontinue use of health care system
§ pain control
Treatment Outline
Acute (0-4 weeks);
§ rule out serious problems
§ short course of bedrest
§ posture connection exercise
§ lumbar support
§ decrease painful/inflammation/spasm
§ keep them active
§ some pain is okay
§ teach patient what to avoid
Subacute (1-10 weeks)
§ increase mobility
§ strength, flexibility, and fitness
§ body mechanics training
§ back care education
§ work stimulation
§ posture training
§ evaluate work environment
§ return to work
Acute/ Subacute pain
§ cold packs, hot packs
§ bed rest
§ simple analgesics
§ massage
§ TENS/US
§ Corset/brace
§ Pelvic traction
§ Manipulation
§ Early activity
§ Back exercises
Chronic (after 7-10 weeks)
§ increase work simulation
§ increase strength, flexibility, fitness
§ rehabilitation psychology
§ behavior modification
William’s Flexion Exercise
1. pelvic tilt
2. single and double knee to chest
3. partial and full sit ups
4. Straight leg raises
5. hurdle’s position
6. wall slides
McKenzie Exercise
1. side gliding
2. forward bending
3. passive prone extension
*on elbows
*on hands
4. Knees to chest while supine
5. prone lateral shifting of the hips off midline
6. backward bending
7. flexion while sitting
8. slouch-over correct
Low Back Hygiene
1. During prolonged sitting
· get up every 2o minutes
· perform pelvic tilt exercise
· sit with knees bent
· one or both feet slightly elevated
2. Driving
· bring seat close to steering wheel
· knees slightly higher than the hip
· stretch every 20-30 minutes
3. Before coughing or sneezing
· tighten abdominal muscles
4. Begin progressive low back isometrics and stretching
5. Bend knees when picking an object from the floor
6. When getting into bed, sit on the edge of the bed, turn and roll to one hip, bring knees up and slowly recline.
Prevention of recurrence of LBP
Objective: Pain Reduction
Exercise suggested for pain reduction and or pain and elimination are supine lumbar flexion prone lumbar extension, side lying, rotation lateral glides and prone lying oscilition.
Objective: Restoration of function
Exercise suggests for the restoration of function are supine lumbar flexion, prone lumbar extension hams stretches, hip flexion stretch, sitting rotation, side lying relation, lateral glides.
Objective: Prophylaxis
Exercise suggested for prophylaxis are supine Flexion, prone ext, hams stretches, hip flexion, stretches, prone rotation, abdominal strengthening exercise paraspinal and gluteal strengthening exercises.
REFERENCES:
Randall L. Braddom. “Physical Medicine and Rehabilitation 3rd Edition”
Joel A. Delisa. “Physical Medicine and Rehabilitation Principles and Practice 4th Edition”